Stop Rubbing
Case Study: Intermittent Diplopia in the Elderly
Dr Elaine Wong
Presentation
4 yo boy present with bilateral red, sore, itchy eyes for 4 months. He has been rubbing his eyes extensively and was prescribed chloramphenicol, cromolyn sodium, olopatadine and oral antihistamine by local doctor with no improvement. In recent weeks, he has also become very light sensitive.
There is a family history of allergic conjunctivitis. Father has reduced vision due to steroid induced glaucoma requiring glaucoma filtration surgery at the age of 8 yo.
Clinical findings
- visual acuities are 3/4.5 OU (Kay Pics)
- IOP of R 13 L 12 (iCare)
Anterior examination

What is this?
The appearance of white dot along the limbus is consistent of Trantas dots. These dots are due to infiltration of eosinophils and epithelial debris.
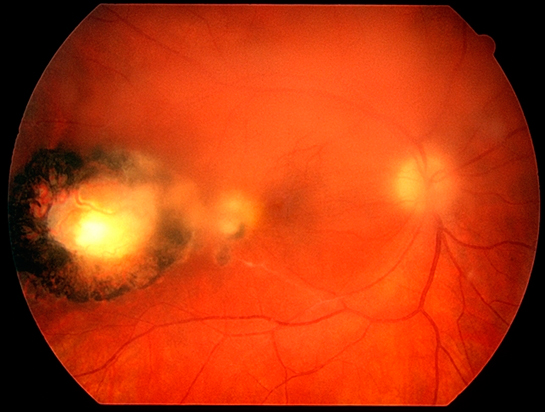
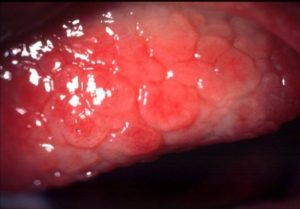
On lid eversion (which was difficult in a 4 yo and photos is of another patient). He was found to have giant papillary conjunctivitis GPC.
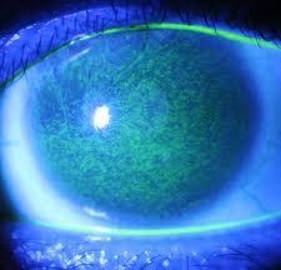
Fluorescence staining show extensive superficial punctate keratopathy.
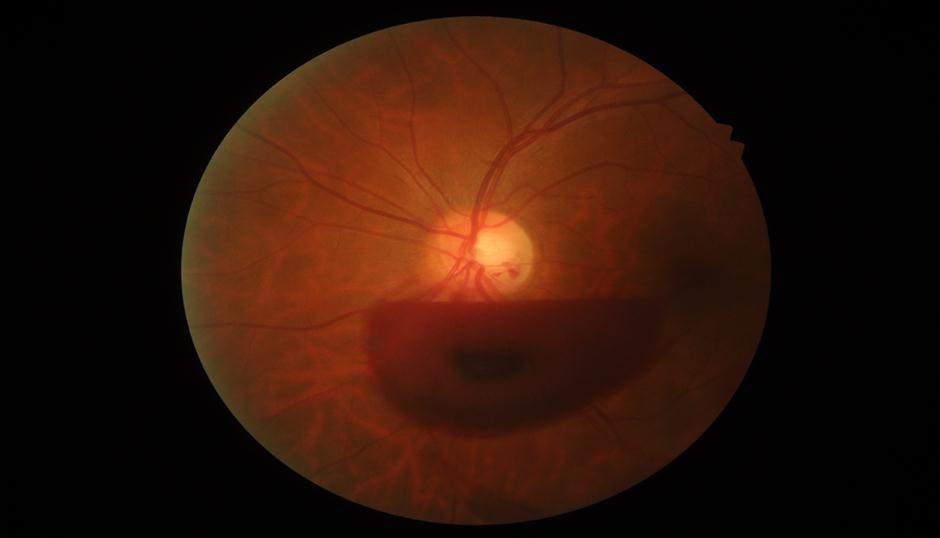
Fundus examinations are normal. Cycloplegic retinoscopy show no significant refractive error.
What condition is this?
The clinical presentation is classic of vernal keratoconjunctivitis (VKC). Vernal Keratoconjunctivitis is an allergy with recurrent inflammation predominantly found in young males age between 5 – 20 yo. Males are twice as likely than female to have the disease. There is usually history of other atopy such as asthma, rhinitis or eczema. It seems to be worse in warmer and dryer climates.
What to do next?
Given this 4 yo has tried both topical and oral antihistamines and mast cell stabilizers, the next line of treatment will be with topical steroids. Given he has significant symptoms, I will start him on a strong steroid such as Prednefrin Forte QID first. Usually, patients with this condition will response very well and symptoms improve within a few days. Once symptoms completely resolve, I will reduce the Prednefrin Forte while re-starting the patient on topical antihistamine eyedrops as prophylaxis. Unlike topical steroids which can give rise to cataracts and glaucoma, topical antihistamines are safe to use in the long term.
The symptoms of this patient resolved and we tapered him off topical steroids but remain on both oral and topical anti- histamine. However, 4 weeks later, he presents again, but this time with reduced vision and inability to open eyes.
This time he was found to have VAR 6/12 VAL 6/18 with IOP of R 12 L 13.
Examinations were extremely difficult and he could barely open his eyes.
With fluorescence staining, you can see a large central corneal ulcer.
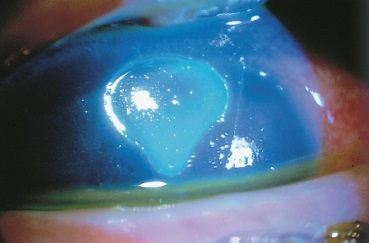
What is this?
This is a Shield Ulcer, a name given due to its appearance often resembling a shield.
What do you do now?
Shield ulcer can be found in up to 10% of VKC. If not treated appropriately, this can lead to corneal neovascularisation and permanent corneal scar.
With the appearance of shield ulcer, I then started him on Chloramphenicol ointment QID and Prednefrin forte 2 hourly. He needed regular review until complete resolution of the ulcer.
Once the ulcer has resolved, I will then reduce his steroid eyedrops. However, with previous experience, rather than stopping his steroid eyedrops completely, I will keep him on a small maintenance dose of weaker steroids such as fluorometholone once to twice daily.
It is important to remember that any steroids can induce glaucoma and cataracts. Therefore, it is important to have constant monitoring. It has been estimated that up to 50% of children on topical steroids can have elevated IOP.
Fortunately, for this child, he never develops cataracts or raised IOP with long term use of steroids. Otherwise, we will have to consider steroid sparing agent such as cyclosporine to control his severe vernal keratoconjunctivitis.
VKC is usually a self-limiting disorder, typically lasts for 4 to 10 years with remission around puberty. But until then, I will be seeing him every 3-4 months to ensure he is not developing glaucoma or cataracts whilst on a low maintenance dose of steroid.